The Cycle of Addiction: Are You in It?
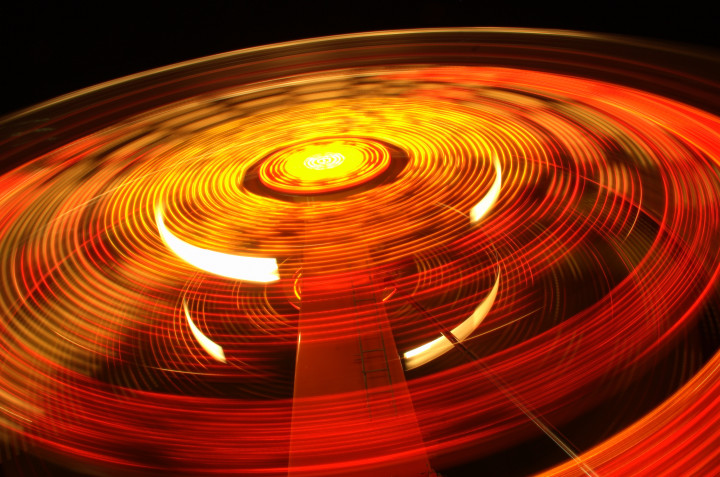
The cycle of addiction is the repetitive pattern people with addiction often experience. It happens in certain stages or phases, but the specifics of the cycle vary depending on the substance or behavior involved. Key Features of Addiction Not sure whether you or a loved one are addicted? Here are a few of the key features of addiction: Not everyone who suffers from addiction shows signs. If you think you or a loved one has an addiction, getting help right away is the best course of action. It’s incredibly hard to break the addiction cycle on your own. The Cycle of Addiction Stages This is definitely the point at which professional help can be helpful. It is so difficult to stop using drugs and alcohol on your own. With a team of people to help you, you can build the skills you need for lasting recovery. This cycle can become a continuous loop, making it difficult to break free from the grips of addiction. But with appropriate treatment and support, many people recover and manage their addictions effectively. If you’re struggling with addiction, it’s essential to seek help. Early intervention can improve the chances of successful recovery. How to Get Out of the Cycle of Addiction Breaking the addiction cycle is challenging, but it’s possible with determination, support, and the right treatment center guiding you. Here are eight ways to help you or someone you know break free from the cycle of addiction: If you’re experiencing negative consequences of addiction or you’ve hit rock bottom, don’t wait to reach out to an addiction treatment facility like Footprints to Recovery. Continuing to use alcohol or drugs could have a devastating impact on your life that you can avoid with treatment. What Does Formal Addiction Treatment Look Like? Formal addiction treatment involves structured and specialized programs that address substance use disorders and other addictions. These treatment programs are overseen by clinical professionals with the proper licensing and credentials. Treatment can involve residential care, where you live full-time at a recovery facility, or outpatient programs, where you live at home but attend treatment regularly as set by your therapist. There are stages of addiction treatment. Before beginning, you undergo a thorough assessment to determine where you are in the cycle of addiction, any co-occurring disorders you have, and your overall health status. This evaluation helps tailor a personalized treatment plan to your needs. For those with substance use disorders, detox may be a necessary part of recovery. Various forms of therapy are used in drug addiction treatment. These commonly include: These therapies address the underlying factors that contribute to your addiction and help you develop coping strategies and healthier behavior patterns. Your therapist may also use psychotherapy techniques like individual therapy or group therapy as part of your recovery program. In some cases, medication may be prescribed to help manage cravings, reduce withdrawal symptoms, and support recovery. Medication-assisted treatment (MAT) is often used in combination with counseling and therapy. Addiction Treatment at Footprints to Recovery The best way to break the cycle of addiction is to get professional help for a substance use disorder. Alcohol and drug rehab is a place where you can focus all your attention on achieving sobriety. The clinical team at a drug and alcohol rehab center like Footprints to Recovery can help guide you through the stages of addiction until you reach your goal of sobriety. Our substance abuse treatment programs are safe and effective for everyone who needs help with addiction. Our levels of care offer a personalized approach to treatment to suit your needs. They include: Footprints to Recovery is committed to treating addiction with dignity and compassion. Drugs and alcohol are powerful substances that create a vicious cycle of abuse. A professional clinical team can help you understand the cycle and break free from it. Addiction recovery starts with contacting the behavioral health admissions team at Footprints to Recovery to learn more about our alcohol and drug rehab programs and to verify your insurance. Don’t wait to get help for substance abuse and mental health issues. Footprints to Recovery can help you break free of the cycle. References: Author Evan Gove
What Is the Pink Cloud?

Why You Need to Know About the Pink Cloud The first few days of sobriety can be overwhelming. Some face difficult withdrawal symptoms. Others face intense cravings for the substance they abused. Getting through these first steps is hard, but it’s necessary for a brighter future. After the initial discomfort, some people in recovery enter a period of improvement known in the addiction treatment community as “the pink cloud” or “pink cloud syndrome.” It’s the feeling that nothing can stop their progress and that relapse isn’t possible. Quitting drugs and alcohol is something to be celebrated, and many people in early recovery feel extreme motivation to continue forward. But addiction recovery is a lifelong process. If you let initial success cloud your judgment on the difficulty of the road ahead, you could be setting yourself up for a relapse. Working with a professional addiction treatment center like Footprints to Recovery can help manage expectations and keep you focused on a brighter future. What Is Pink Cloud Syndrome? There’s something special about getting sober. Those who get through detox and move on to residential or outpatient treatment are often brimming with confidence about their situation. Feeling overly happy and motivated during this period is a phenomenon known as the pink cloud. It’s when you feel extra motivated to pursue your recovery due to the great feelings that come with initial sobriety. The problem is that these feelings can fade as you progress, which could open the door for a relapse as mental health issues like depression, anxiety, and stress creep back in. The idea of a pink cloud period started with those in Alcoholics Anonymous (AA). People in meetings for alcoholism began seeing members exude positivity during the start of their sobriety. It’s often described as being “high on life.” Some of the signs and symptoms of pink cloud syndrome include: What Is Dangerous About Pink Cloud Syndrome? Feeling good can’t be dangerous, right? It feels like positivity and confidence in sobriety are a good thing. Unfortunately, that isn’t the case with the pink cloud. The danger of the pink cloud phase comes not in the feelings of happiness and euphoria but in the actions you could take as a result of those feelings. Here are some of the reasons why the pink cloud can be dangerous and lead to a relapse: At its core, the pink cloud is an obstacle in recovery that some people need to deal with. Ending treatment too early or not following through with aftercare programs can send you right back to square one with your substance use disorder. Does the Pink Cloud Cause Relapse? Many factors can cause a relapse. Pink clouding can certainly be included on that list. The false confidence it instills can be very dangerous because the recovery journey is not easy. The pink cloud can cause you to neglect your recovery and fall back into old patterns of substance abuse and addiction. Some other factors that can play a role in drug or alcohol addiction relapse include: Tips for Preventing Relapse Relapse prevention is hard. It takes effort and commitment to remain sober even when life’s triggers and stressors cause problems. The best way to prevent relapse is to work with professional treatment programs with certified and licensed counselors. Footprints to Recovery offers a full continuum of care, from detox through aftercare services. Our team of counselors can help you manage expectations and set achievable goals as you progress through the recovery process. Other tips for preventing a relapse include: Avoid the Pink Cloud with Footprints to Recovery The goal of an alcohol and drug treatment program is to provide you with the skills and tools necessary to not just reach sobriety but maintain it long into the future. Recovery programs like those at Footprints to Recovery consider factors like a co-occurring disorder, which can complicate addiction. Our addiction and behavioral therapy programs make our recovery center a great option for everyone. Footprints to Recovery offers unique levels of care and individualized treatment programs that can aid in long-term recovery and reduce your risk of relapse. Medical detox: The first step in getting sober is to stop using drugs and alcohol. This often means undergoing a detox period. Footprints to Recovery has a safe and comfortable detox facility operated by our team of substance abuse treatment professionals. We can help reduce difficult withdrawal symptoms so you can move on to the next phase of recovery. Residential treatment: After detox inpatient care is an option if you’re looking for the most structure and guidance in your recovery program. Residential treatment involves living full-time at our treatment facility while you undergo treatment every day. You’ll avoid triggers while you gain valuable tools and coping skills to aid sobriety in your future. Partial hospitalization program (PHP): Partial hospitalization is outpatient rehab that still offers structure for those in need. You attend treatment every day while living at home or a sober living home when not at our facility. A PHP is the start of your transition back to normal life. Intensive outpatient program (IOP): An IOP is similar to a PHP in that you don’t live full-time at a treatment center. It features 9 to 15 hours of treatment per week, depending on your needs. The goal is to build on the skills and tools learned in recovery to aid long-term sobriety. Outpatient rehab: Outpatient treatment is a form of therapy that involves attending programs at our recovery center just once or twice per week. An outpatient rehab program will help you learn to manage your addictions and avoid triggers to remain sober in the future. At Footprints to Recovery your treatment plan is tailored to meet your specific needs and goals. It considers the important components of your life, such as living environment, family dynamics, work obligations, and realistic time commitments. We can help you detox, make it through the pink cloud phase of recovery, and prevent relapse in the future. Contact us
What Is a 12 Step Program for Addiction?

The statistics surrounding drug and alcohol abuse in the United States are cause for concern. According to data from the National Center for Drug Abuse Statistics, close to 100,000 Americans die from drug overdoses each year. Opioids, a class of prescription drug used for pain management, account for close to 68% of drug overdose deaths. Alcohol use is also problematic. A 2021 survey from the Substance Abuse and Mental Health Services Administration found that nearly 30 million Americans over the age of 12 suffered from alcohol use disorder in the past year. Substance abuse affects everyone differently. Some may notice when casual drug or alcohol use turns into something more and take steps to curb their addiction issues. One of the most common ways people find help for addiction is through 12 step programs. These programs are peer-led and offer a safe space where anyone can share their experiences with recovery. Twelve-step programs can be valuable to the recovery process, but they don’t offer the same level of care a professional treatment center does. Footprints to Recovery’s full continuum of care for addiction and mental health disorders is rooted in compassion and dignity for all. We offer a variety of holistic and evidence-based treatment methods for an integrated approach to recovery. Our team of addiction professionals is dedicated to providing unparalleled support, guidance, and care to those in need. What Is a 12 Step Program? There are different avenues you can take for addiction recovery. The most advisable method is to get help from a professional substance use disorder treatment center. Another popular option is using peer support groups to aid in the recovery process. Twelve-step programs are peer-led groups that provide support and shared experiences. They have helped many people on their journeys to end serious addiction problems. According to research, those who attended 12 step groups following treatment fared better in their recovery journeys. As the name implies, many of these groups outline 12 traditions or steps you must take to complete the recovery process. After finishing the steps, your attitude toward substance abuse may have changed, allowing you to focus on sustained sobriety. Twelve-step program meetings provide members with safe spaces for sharing. You can also develop friendships and receive emotional support from your peers in recovery. The main difference between a recovery center and a 12 step program is that those who oversee peer-led programs may not be licensed and certified addiction treatment counselors. Seeking treatment from a professional facility means you receive comprehensive care overseen by treatment staff. These are people who are capable of providing medically assisted treatment and more. Peer-led groups are more focused on sharing experiences and finding common ground than providing integrated treatment. Popular 12 Step Programs Alcoholics Anonymous (AA) is the original 12 step group. The model proved effective in treating other addictions as well, which led to the formation of many different specific addiction 12 step groups. These recovery groups can be found all over the country. Some of the most popular 12 step groups include: Some groups get even more specific. While Narcotics Anonymous is a group for general drug use, there are specific groups that meet for some drugs. Those include substances like: The sense of community and support from others is often crucial in treatment as you can come to realize you aren’t alone on your journey to a brighter future. Research has shown that those who participate in 12 step groups have lower rates of substance use and fewer alcohol- or drug-related problems as a result. The study also found that people looking to overcome drug addictions using 12 step programs may have a more difficult time than those who seek help for alcoholism. What Is Alcoholics Anonymous? AA is a 12 step program offering support to people struggling with an alcohol use disorder (AUD). The program was first used by Bill Wilson and Dr. Bob Smith in 1935 in Akron, Ohio. The main premise of the group is that alcoholics are powerless in their fight against alcohol abuse. To reach lasting sobriety, you need to put your faith in a higher power and take a moral inventory of yourself. An AA meeting is a regular weekly event with a set time and location. Many who have completed formal alcohol dependence treatment find that attending 12 step meetings like AA aids in their ability to resist the urge to drink. There’s a motivational enhancement aspect to sharing recovery stories that can help you feel confident in your recovery journey. A volume known as “The Big Book,” first published by the group’s founders, provides a guideline for those looking for help with their drinking. The Big Book outlines the principles and philosophy of AA and presents a 12 step program for recovery from alcoholism. The 12 steps are a series of principles and actions individuals can follow to achieve sobriety and maintain their abstinence from alcohol. The Book also includes personal stories of people who have successfully recovered from alcoholism through the AA program. The twelve steps are the same for AA, NA, and other behavioral programs for addictions like gambling or sex. The 12 steps of Alcoholics Anonymous are: There is no set timeframe for how long AA takes. That process is different for everyone. AA is a self-help fellowship that provides ongoing support for people in recovery from alcohol addiction. Participants can engage with AA for as long as they find it helpful to their sobriety journeys. Factors such as the severity of your addiction, your desire to achieve sobriety, and your past history of recovery attempts can all affect how long you attend AA meetings. In some cases, people attend meetings for the rest of their lives to continue their goal of long-term sobriety. What Is Narcotics Anonymous? NA is an international, community-based organization that provides support and a structured program for those struggling with drug addiction. It follows a similar model to Alcoholics Anonymous but is tailored to address the needs
Bipolar Disorder and Addiction

Bipolar disorder is a well-researched mental health condition. As far back as the Ancient Greeks and Romans, humans have noticed each other experiencing episodes of mania and depression. Between 4% and 5% of American adults will experience bipolar disorder at some point in their lives. It wasn’t until the 1950s that the first formal diagnosis of manic-depressive disorder appeared in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-I). The In 1980 the term bipolar disorder was used for the first time. Today bipolar disorder is a treatable mental health disorder that often appears as a co-occurring disorder with substance abuse. The extreme shifts in mood that come with bipolar are only one of the reasons why there are such high rates of substance abuse among those who suffer from bipolar disorder (40%). Footprints to Recovery is a valuable resource if you want to overcome your struggles with co-occurring bipolar disorder and addiction. Our team of behavioral health and substance abuse treatment clinicians have helped countless people regain control of their lives, and we’re ready to help you. What Is Bipolar Disorder? Bipolar disorder is a diagnosable mental health condition that causes extreme mood swings or episodes of mania and depression. These mood swings can be severe and disrupt your normal life. Each episode can last for days, weeks, or months. This can lead to difficult periods in your life when simple things like family responsibilities, school, or work become far more challenging. There is no cure for bipolar disorder, but with proper management and treatment, you can control your symptoms for a happy and fulfilling life. Different Types of Bipolar Disorder Researchers have pinpointed different types of bipolar disorder while studying the condition. The main difference between them is the severity of symptoms. Each diagnosis comes with a unique treatment and recovery plan set forth by a treatment center like Footprints to Recovery. The different types of bipolar disorder are: Another form of the disorder, called unspecified bipolar disorder, is also used for those with symptoms that don’t fall exactly into one of the above types. What Are the Symptoms of Bipolar Disorder? Bipolar disorder features two unique moods that have very different symptoms and treatment needs. The two sides of bipolar disorder are mania and depression. The symptoms of each are below: Manic Episode Symptoms: Depressive Episode Symptoms: What Causes Bipolar Disorder? The exact cause of bipolar disorder is not known. Many believe it involves a combination of genetic, biological, and environmental factors. Most researchers agree that a complex interplay between factors contributes to the disorder. Some of the factors that may play a role in bipolar disorder include: Why Do People with Bipolar Disorder Self-Medicate? Self-medicating is a dangerous but common practice. It’s when you use drugs or alcohol to reduce the symptoms associated with mental illness. Issues like depression or anxiety are commonly associated with substance abuse. Unfortunately, bipolar disorder is as well. According to a study, more than 40% of bipolar I and bipolar II patients suffer from life-long substance abuse disorders. Research is still trying to understand the full link between bipolar disorder and addiction, but many experts believe self-medication plays a role. Using drugs and alcohol may offer temporary relief, but substance abuse does not treat mental health disorders, and it certainly doesn’t cure them. It may be the opposite. Drug and alcohol use can alter the chemistry of your brain and nervous system. It also affects the reward system in your brain, causing pleasure-seeking behavior. Some other reasons why those with bipolar disorder are more prone to addiction include: Alcohol is problematic for those with bipolar disorder because it’s so readily available. Drinking alcohol can help reduce manic and depressive symptoms in the short term, but long-term alcohol use is harmful. It also opens the door for physical dependence. This means you need more alcohol to feel good. Abusing alcohol to self-medicate can also make bipolar symptoms worse. Breaking the cycle of using drugs or alcohol to feel better is critical for treating bipolar disorder. And finding a treatment plan that works is an important step in the process. Treating Co-Occurring Bipolar Disorder and Addiction When you’re dealing with both bipolar disorder and substance abuse, it’s known as a dual diagnosis. Treating co-occurring disorders isn’t something you can do on your own. Simply detoxing from alcohol or other drugs isn’t enough. Treatment for a dual diagnosis should be done by professional behavior and substance abuse counselors at a certified addiction treatment center. That’s because these addiction and mental health professionals know understand integrated treatment—treating both issues at the same time. Only treating one opens the door for relapse and a return to the cycle of mental health issues and addiction. Here are some of the ways bipolar disorder is treated, which can be incorporated into drug addiction treatment as well: Medication Management Medication is a common way of treating bipolar disorder. Bipolar medications include: The team at Footprints to Recovery can help with medication management for bipolar disorder. When you enter our facility, our team of licensed and professional therapists will conduct a thorough evaluation to determine if medication is right for you. Finding the right balance with medications is key for successful treatment. It may take some time for your doctors to find the correct medications and dosages for effective treatment. Why Some People with Bipolar Don’t Stay on Their Medication It’s not uncommon for people with bipolar disorder to stop taking their medications. The reasons often include: When you partner with a treatment facility like Footprints to Recovery to treat your bipolar, we’ll work with you to find the best treatment path for your situation and your preferences. Our goal is to get you feeling well, no matter how long it takes. Psychotherapies Talk therapy is one of the most effective ways to treat a mental health disorder. There are many different forms of psychotherapy, and they all have certain goals and benefits. Here are some of
Trauma and Addiction: What’s the Connection?
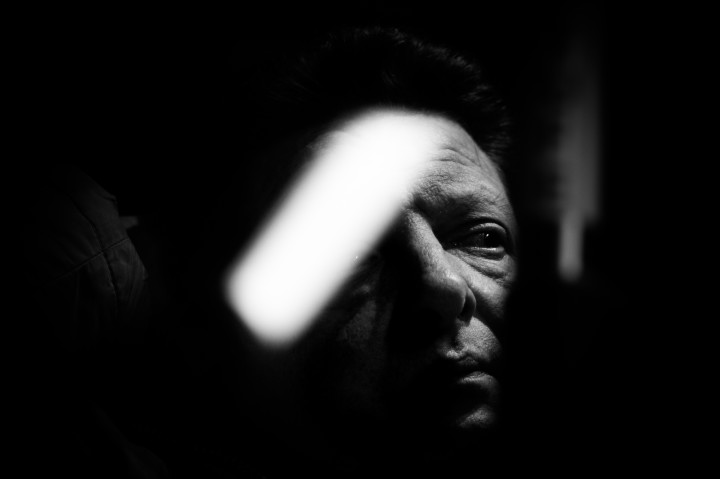
Footprints to Recovery offers treatment for trauma and addiction that is rooted in compassion and dignity. Our clinical team can help you recover from co-occurring disorders and move on to a brighter future. Your experiences in life shape who you are. If those experiences are traumatic, they can lead to a serious mental health condition known as trauma. Living with trauma is a challenge, but thankfully there are treatment programs available to help with the healing process. What Is Trauma? Trauma is the term used to describe distressing or disturbing experiences or events that overwhelm a person\’s ability to cope. These situations leave lasting emotional, psychological, and sometimes physical effects long after they’re over. Traumatic events can be single incidents or ongoing situations that cause harm to someone’s mental and emotional well-being. Trauma is different for everyone. What one person finds traumatic may not be perceived the same way by someone else. Some examples of situations that cause trauma include: The list above features a few common examples. There are countless other situations and incidents in life that could cause trauma. What Are the Signs and Symptoms of Trauma? The symptoms of trauma can vary from person to person, depending on the nature of the traumatic experience and their individual coping mechanisms. Trauma can affect people emotionally, psychologically, and physically. Some common symptoms of trauma include: What Are the Different Types of Trauma? When discussing trauma, the condition is divided into three distinct categories: Acute Trauma Acute trauma refers to a sudden and intense event or experience that poses a threat. This type of trauma is often unexpected. You may feel overwhelmed and unable to cope with the situation. Acute trauma can result from various incidents, such as: Chronic Trauma Chronic trauma refers to repeated exposure to traumatic events or stressful situations. These occur over an extended period of time. Unlike acute trauma, which is characterized by a single intense incident, chronic trauma involves ongoing stressors that can be interpersonal, environmental, or systemic. Examples of prolonged situations that can cause chronic trauma include domestic violence and military service. Complex Trauma Complex trauma is a psychological condition that results from experiencing prolonged and repetitive traumatic events. It’s also known as complex post-traumatic stress disorder (C-PTSD). It often occurs during childhood or early developmental stages of life. It is a more severe and chronic form of trauma compared to single-incident traumas or acute traumas. Complex trauma often occurs in interpersonal relationships, where you are subjected to ongoing abuse, neglect, or abandonment. Trauma and the Brain Trauma can have a significant impact on the brain. It can affect the brain’s structure, function, and neurochemical balance. When you experience a traumatic event, your brain responds in order to cope. In cases of severe or prolonged trauma, these responses can lead to changes in the brain. Trauma can affect the following parts of the brain: Amygdala: The amygdala is a part of the brain responsible for processing emotions. These include fear and threat detection. During traumatic experiences, the amygdala becomes hyperactive, leading to heightened emotional responses and being especially aware of potential dangers. This can mean you get triggered by reminders of the trauma. Hippocampus: The hippocampus plays a crucial role in forming memories and consolidating them. Trauma impairs the hippocampus, leading to difficulties in processing and integrating memories of the traumatic event. This can result in fragmented or intrusive memories, contributing to symptoms like flashbacks and nightmares. Prefrontal Cortex: The prefrontal cortex is involved in decision-making, impulse control, and emotional regulation. Trauma can affect the prefrontal cortex\’s function, leading to difficulties in managing emotions and making sound judgments. This can contribute to impulsive behaviors and emotional dysregulation. Neurochemical Imbalance: Trauma can disrupt the balance of neurotransmitters in the brain, such as serotonin and dopamine. These are crucial for mood regulation and pleasure, and an imbalance can contribute to symptoms of depression, anxiety, and other mood disorders. Effects of Childhood Trauma Childhood trauma can have long-lasting effects on your development, emotional well-being, and physical health. Adverse childhood experiences such as child abuse, neglect, and parental loss can lead to a range of trauma symptoms in adulthood. According to the Substance Abuse and Mental Health Services Administration, 2 out of 3 children experience a traumatic incident by the time they reach 16 years old. Childhood trauma has been linked to many adverse effects including: The Connection Between Trauma and Addiction There is ample evidence that mental health disorders like trauma play a role in developing and continuing substance abuse. In turn, substance abuse can make the symptoms of trauma more severe. This cycle of co-occurring disorders can be a nightmare to escape from. The cycle begins when someone experiences a form of abuse or trauma. After experiencing this kind of stressor, they may turn to drugs and alcohol as a way to cope with their emotions and negative thoughts. Substance abuse serves as a temporary escape from their problems, but it creates a new issue in the process. Can Trauma Cause Addiction? Trauma can be a significant factor in developing a substance use disorder. When someone experiences trauma, it can have a lasting impact on their emotional health. Trauma can lead to mental health issues such as anxiety, depression, and emotional pain. Some trauma survivors may attempt to reduce these feelings through substance use to self-medicate or escape distressing emotions. It is important to note that trauma does not necessarily cause addiction. There are cases where someone experiences trauma and does not develop a substance use disorder as a result. The reverse is also true. While addiction can make symptoms of trauma worse, those who abuse substances may not necessarily have experienced trauma in their lives. While it’s not fully accurate to say that addiction causes trauma or trauma causes addiction, the relationship between the two cannot be ignored. Both are complex mental and behavioral health issues that can make each other worse if left untreated. Finding reliable mental health and substance abuse treatment is
Tramadol Addiction: Is It Possible?

Tramadol is an opioid medication often used for pain management. Its brand names are Ultram and Ultram ER. But prescription drug addiction also carries a high risk of abuse and physical dependance because of how drugs affect brain chemistry. Tramadol addiction can take hold quickly but there are solutions. Prescription opioid are synthetic drugs created in labs to mirror the effects of opiates, a kind of drug that comes from the poppy plant. For thousands of years, various cultures have used opiates for their pain-reducing qualities. Tramadol was first approved in 1995 by the U.S. Food and Drug Administration. About 20 years later it became a controlled substance under the Controlled Substances Act. Tramadol can be ingested in tablet form (most common) or injected intravenously. When prescribed by a doctor or pharmacist and used in an effective dose, tramadol can treat moderate to severe pain. But misusing tramadol can have serious consequences. When people take tramadol in doses higher than prescribed, they risk dependency. They may also experience withdrawal symptoms if they try to stop. This is how how tramadol addiction can start. Long-term abuse of opioids like tramadol can damage organs and increase the risk of overdose or even death. How Addictive Is Tramadol? Tramadol is a powerful synthetic opioid that carries a significant risk for addiction and abuse. It may not be as potent as other opioids like OxyContin or Vicodin, but it still acts on the brain’s opioid receptors at a chemical level. It also affects the central nervous system. When used to treat severe pain, tramadol inhibits feelings of pain by releasing endorphins in the brain. This provides an analgesic effect and temporary relief. But once the drug wears off and its pleasurable effects are gone, cravings, drug-seeking behavior, and abuse can occur. Prolonged use of Tramadol carries an increased risk of overdose and death due to its potency. Opioids are even more dangerous when combined with other drugs or alcohol. The reaction between opioids and medications like antidepressants or migraine treatments can lead to serotonin syndrome. That is when too much serotonin hits the brain at once. Symptoms of serotonin syndrome include: This makes it especially important not to combine opioids like tramadol with other medications that can cause increased serotonin reuptake, such as herbal products like St John’s Wort. It is important to tell your doctors about any medicines you’re taking before taking opioids like tramadol. The risks associated with tramadol use become even more serious when combined with alcohol, including: If you are a frequent drinker, speak to your doctor before taking tramadol. Never ignore potential side effects. Seek medical help immediately if you experience dangerous symptoms after combining drugs and alcohol. Doing so may save your life. Signs and Symptoms of Tramadol Addiction Seeing a loved one battle the effects of addiction to tramadol is heartbreaking. Opioid abuse can be extremely dangerous and cause serious health complications, even when taken as prescribed for pain relief. Intervention is critical in the fight against opioid abuse and dependence to prevent serious side effects. The longer someone uses an opioid like tramadol, the more difficult their addiction can be to treat. Getting help as soon as possible for tramadol addiction is essential for full recovery and long-term health and well-being. Those who think a friend or family member is abusing tramadol should look out for the signs and symptoms of opioid abuse. Here are common signs that someone is suffering from tramadol addiction: Tramadol Addiction Treatment Options at Footprints to Recovery Finding help for a tramadol addiction is crucial because opioid overdose is a very real issue. It can be difficult to know where to turn for help when tramadol threatens your well-being. Footprints to Recovery operates licensed treatment centers in Colorado, Illinois, and New Jersey. The staff is accredited and professional clinical therapists. Tramadol recovery at Footprints to Recovery involves evidence-based treatment programs. These are proven effective at treating tramadol and other opioid abuse. If you use tramadol to treat chronic pain, our therapists can help find alternatives to a dependence on opioid medication. A consultation can determine what levels of care will be most effective in ending tramadol dependence. Medical detox – One of the first steps in the recovery process is ridding the body of all substances. Under the care of medical professionals, you can safely detox from tramadol in a comfortable environment. Detox is part of an overall recovery plan curated by the treatment providers at Footprints to Recovery. With their help, you can get past tramadol withdrawal symptoms. Your plan will be tailored to your needs, helping you find your own unique path to sobriety. Residential addiction treatment – Inpatient treatment offers a comprehensive approach to clinical care that helps you develop the skills and strategies you need to recover from opioid addiction. You can gain insight into your substance use patterns and learn to manage triggers in inpatient rehab through: Partial hospitalization program (PHP) – Clients spend around six hours per day in individualized therapy programs at a treatment facility. The other hours of the day are free for you to pursue normal daily activities, such as school or work. This allows you to remain connected to your existing support systems. The focus remains on long-term healing. Intensive outpatient program (IOP) – IOP helps you transition back into your everyday life from intensive treatment for tramadol addiction. Through this program, you can gain the vital coping skills to handle triggers when they come up. You will attend meetings or therapy sessions a few times per week to learn how to better manage your thoughts and behaviors. With these tools and resources, you can improve your mental health and get a more positive outlook on life without the threat of substance use disorders. Outpatient rehab – Outpatient treatment allows a more gradual transition back into your own life. Clients usually attend treatment once or twice per week. The caring team of treatment counselors is available at all times. They
Personality Disorders & Drug or Alcohol Addiction

People who deal with drug or alcohol abuse and have a personality disorder can still get help and live healthy, productive lives as long as treatment adequately addresses both conditions. Integrated care that treats both issues simultaneously is key to long-term stability. Personality disorders are not flaws of character or eccentric qualities. These are disorders that prevent you from thinking in healthy and functional ways. Individuals with a personality disorder are not always aware they are dealing with one because they believe their thinking or behavior is normal. Most personality disorders show up in the teen or young adult years. They can hinder a person’s ability to reach their potential and cause problems forming appropriate relationships. The National Institute of Mental Health says that up to 9.1 percent of Americans may have one of the personality disorders. Types Of Personality Disorders The most recent version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) says there are 10 distinct personality disorders. Studies show that people with personality disorder may also meet the criteria for another one. The DSM-5 also separates personality disorders into three clusters, as follows: Research shows that family history may contribute to the development of cluster B disorders, which include: An estimated 1.4 percent of Americans are affected by borderline personality disorder (BPD). More than any other personality disorder, people with BPD are likely to face co-occurring issues, such as other anxiety disorders, substance use disorders, mood disorders, and impulse control disorders. Getting A Diagnosis Diagnosing a personality disorder is challenging because a lab, blood, or other conventional test cannot confirm or deny its presence. These tests can still be valuable in ruling out other medical conditions that cause unusual behaviors. As a result, doctors may run these during the assessment phase of care. Doctors will also take down a patient’s family and medical history. Patients are then referred to a psychiatrist or psychologist if doctors find no physical cause for the behaviors displayed. A mental health practitioner can then evaluate a patient and use the DSM-5 to assess whether they fit the criteria for any of the personality disorders described above. How Drugs & Alcohol Are Linked With Personality Disorder A 2011 study published by Innovations in Clinical Neuroscience found that substance use disorders are common in people with personality disorders. People with BPD are especially at risk of a substance use disorder. The study says the link between BPD and substance misuse is strong, and patients are most likely to abuse prescription medication. The study also found that: Why Is Substance Abuse More Likely? As explained by the National Institute on Drug Abuse (NIDA), drug addiction is a mental illness because it changes the way a person’s brain works, shifting their priorities, decreasing their ability to control impulses, and developing a new hierarchy of needs. A person who deals with substance misuse and a mental health or other chronic condition is said to have a co-occurring disorder or dual diagnosis. Data shows that mental health issues and substance abuse are linked in the following ways: Treating a co-occurring personality disorder can be a challenge because habitual drug use can also trigger mental health conditions, making it hard to pin down the cause of a mental illness. In addition, prescription medication can cause behavioral changes that resemble those of a personality disorder. Treating Co-Occurring Disorders The good news is that people with co-occurring disorders can find help and lead productive lives, regardless of the root cause of the disorder. You are not alone if you deal with co-occurring disorders. The National Alliance on Mental Illness (NAMI) says that up to 9.2. million adults dealt with co-occurring substance use disorders and mental illnesses in 2018. Per the National Institute on Drug Abuse (NIDA), effective treatments for substance use disorders: Common methods used in treatment programs for co-occurring disorders include: A Path Forward in Recovery Integrated treatment is the key to sustained recovery from personality disorders and substance abuse. Choose a treatment facility that offers a holistic approach to recovery, treating patients on all fronts. If only one issue is treated, it’s highly likely that symptoms of the other disorder will lead to relapse of the treated issue. When it comes to co-occurring disorders, you can’t achieve recovery unless you address the whole person. Treatment won’t separate each disorder. Instead, both disorders will be simultaneously addressed in therapy sessions. As a result, patients see progress in all areas of life, and this leads to lasting recovery.
Opiate vs Opioid: What’s the Difference?

If you\’re familiar with the current opioid epidemic in the United States you have most likely heard the words opiate and opioid. Have you been asking yourself what is an opioid vs opioid? More than 8 million people abused prescription pain medication in the past 12 months. That number has led many people to call the abuse of these medications a public health crisis. While intended to treat pain, these medicines also carry a high risk of misuse. The long-term health implications of prescription medication abuse is also troubling. It can be difficult to watch someone fall victim to pain medication addiction. It can be even more difficult to get them help. What confuses many is the large number of names used to describe these medications. They are often referred to by their manufacturer names, like Percocet or Vicodin, but they can also be called by their generic names, like hydrocodone or fentanyl. You may have also heard them called opiates or also opioids. That leads many to wonder if there’s a difference between an opiate vs opioid. There is a difference, and understanding the difference between opiates and opioids can help you guide a loved one towards the right path to recovery. There is a high risk for opiate and opioid overdose, so getting help right away is important. What Is an Opiate (vs and Opioid)? An opiate is an addictive drug derived from the poppy plant. These drugs include: These drugs are considered natural because they come from a poppy that grows in nature, and some are used for medical purposes. Heroin’s class of drugs, however, is a Schedule I narcotic. That means it has no medical value and it’s highly addictive. Opiates cause feelings of pleasure and relaxation. These drugs are very powerful and affect the brain on a chemical level. This is due to the release of endorphins in the brain when an opiate is introduced to the body. When these feelings go away, it can lead to uncontrollable cravings, impulsive usage, and abuse. Opiates carry a high risk of overdose and death, particularly when abused over a long period of time. What Is an Opioid? Advancements in medical science over the years led to the creation of opioids. They function in a similar way to opiates but are, at least in part, synthetic. That means they are created in labs to mimic the effects of natural opiates. There are more than 500 synthetic opioids with a wide range of uses. For instance, some are used in cough medication to reduce discomfort. Others are prescribed following surgery and accidents to help patients feel less pain. Others, like methadone, are actually used to treat pain medication addictions. Opioid drugs are often prescribed by doctors as pain medicines, but, like opiates, opioids cause feelings of euphoria and pleasure. Over time, users can build up a tolerance so higher doses are needed to feel the same high. That makes their urges to use the drugs worse. When abused, opioids can have serious consequences and have troubling drug overdose death rates. If you are addicted to opioids, it’s important to find help as soon as possible. If left untreated, the risk for overdose or even death will only grow. Opiate vs Opioid: Is Either Safe to Use?
What Is Residential Rehab Like?

Residential rehab is an intensive treatment where individuals stay in a facility for 24 hours a day. It typically lasts 21 days to several months. As the most intensive form of substance abuse treatment, residential rehab is most successful in helping those with severe or long-term addictions. Facilities typically offer group counseling, individual counseling, case management support, family therapy, and other treatment plans. What Is Rehab Like: A Typical Day in Inpatient Treatment The first week of addiction treatment in a residential facility like Footprints to Recovery usually consists of a detox period. This ensures drugs and/or alcohol are out of your system so you can enter treatment no longer influenced by their effects. Detox can often be difficult or dangerous. At a treatment center, professional addiction treatment counselors oversee medical detox so you have support and care throughout the process. These experts help manage withdrawal symptoms, watch your vital signs, offer emotional support, and administer medication. How intense detox is and how long it lasts depends on factors like what substances you abused and for how long. Co-occurring mental health disorders can also affect the severity and duration of withdrawal symptoms. The staff at Footprints to Recovery focus on establishing a safe place for controlling cravings and managing withdrawal symptoms. After medical detox, inpatient rehab is very structured and filled with activities and therapies. This eliminates boredom and downtime, which may tempt you to relapse. Planning the day distracts you from cravings and teaches you how to live differently. Each program varies, but a typical day usually looks like the following: You’ll rise early and have a healthy breakfast. Some facilities offer morning programs such as yoga and meditation. These help you form new healthy habits that can be continued outside of treatment. Afternoons are reserved for therapy sessions. An individual therapy session might include cognitive behavioral therapy (CBT). CBT is one of the most effective methods in substance abuse treatment. According to the National Institute on Drug Abuse (NIDA), it has been effective during treatment and after people leave a facility. This therapy teaches you to anticipate problems and enhance self-control through effective coping strategies. Other forms of therapy may include: In the evenings you’ll have opportunities to engage socially and be a part of sober recreation, like: Or you might choose to read, journal, pray, or meditate. Group Therapy Group therapy is an important and highly effective treatment for addiction issues. It involves mediator-led meetings with others who share your desire to get sober. Meetings are safe and supportive settings where everyone collaborates on how to handle addiction and the issues in life that come with it. Group therapy can help you develop better communication skills and allow you to see that you aren’t the only one who struggles with drugs or alcohol. A sense of community support creates a place where you can feel open and vulnerable as you work towards sobriety. Case Management In residential addiction treatment you’ll be assigned a case manager. Your case manager is part of your system of support during your time at a recovery facility. They’ll also be there for you in the future when you feel like you need help to prevent a relapse or negative decision making. Your meetings may entail creating a treatment plan, connecting you to a provider, and keeping track of your progress. Medication Assisted Treatment Medication, such as methadone, can help treat addictions. The medications should only be used under the supervision of an addiction treatment professional. When taken in a supervised setting, medications can: It is important to understand that these medications do not cure addiction. They are most-effective in addiction recovery when used alongside counseling and other forms of behavioral therapy. 12-Step Model Support/Recovery Groups The 12-step model offers a free, peer-based treatment program for those with drug use disorders. Participants adhere to a set of instructions to refrain from using their preferred substances. Each step is a guiding principle that helps someone avoid triggers, cope with stress, and stay sober even when life gets difficult. The 12-step model involves regular group meetings, which help create a sense of safety, inclusion, and community among attendees. Examples of 12-step recovery groups include: These types of programs are often used during aftercare following residential rehab. Aftercare is an ongoing form of addiction treatment for those who have completed their inpatient and/or outpatient treatment programs. Aftercare offers support and care post-rehab so you can remain on a path to sober living. Pros and Cons of Residential Addiction Treatment It is important to take the pros and cons of residential addiction treatment into consideration before you commit to a level of care. There are benefits and drawbacks to this treatment path, and it may not be the correct process for everyone. Here are some important pros and cons to consider when deciding if residential treatment is right for you. Pros of residential rehab include: • 24-hour medical and emotional support• Medical support during withdrawal symptoms• None of the distractions or temptations of everyday life• Flexible program lengths• Structured programming• Nutritional support• Forming new healthy habits• Sense of community• Establishing healthy boundaries Cons of residential rehab include: • More expensive• Disruptive to everyday life• Limited access to social circle support All the items listed in the pros section are important reasons why you should consider residential rehab over a 12-step program or trying to quit alcohol or drugs at home. The outstanding level of care provided; access to skills development; and the opportunity to turn your life around in a distraction-free, safe environment should be reasons to consider getting help from a professional recovery program. Trying to get sober on your own can be difficult, frustrating, and ineffective. For many, attending occasional meetings isn’t enough to get a grip on their addiction problems. Residential rehab is the more effective treatment for those in search of a sober future. What Are Other Types of Rehab Like? Residential rehab is just one type of addiction treatment offered by
Risks of Home Detox & Quitting Cold Turkey

You’ve made the right decision to take back your life from addiction. Recovery is hard work, but you’ll find it’s well worth it. For people with substance use disorders, the first step in recovery is detoxing from drugs or alcohol. Some people attempt drug or alcohol detox at home, but in many cases, this can be dangerous—even deadly. Learn why the safest way to detox from substances, especially alcohol, is under the 24-hour care of medical professionals. The symptoms of alcohol withdrawal can be intense and, in some cases, life-threatening without medical supervision. According to some research, more than 50% of people going through alcohol withdrawal have symptoms that should be medically attended to. Furthermore, 37% of people who experience delirium tremens (DTs) die. Delirium tremens (DTs) is a life-threatening, alcohol-related condition that causes extreme confusion, hallucinations, and tremors. DTs can occur in people who have been drinking heavily for an extended period of time and can lead to seizures, coma, and death. What is Withdrawal Like? Without medical care, withdrawing from drugs and alcohol can be painful, and cravings may feel unbearable. When you’re addicted to drugs or alcohol, your brain begins depending on substances to function “normally.” When you stop taking drugs, your central nervous system goes into overload as it tries to rebalance itself without the presence of drugs or alcohol. During this process, your brain sends signals and produces chemicals and hormones that cause you to experience withdrawal symptoms and intense urges to use substances again. Drug withdrawal symptoms can range from mild to even potentially life-threatening. Withdrawal from some substances—like opioids, benzodiazepines, and alcohol—can be deadly. Withdrawal symptoms depend on: Withdrawal can include emotional and physical symptoms, such as: Alcohol withdrawal is one of the most dangerous of all substances. During detox, your body rids itself of drugs and alcohol. If you quit drinking or using drugs suddenly—also known as quitting “cold turkey—”you may experience dangerous side effects. Certain medications can help make the detox process more comfortable. A medical professional knows which medications and what doses are best for your individual situation. RISKS OF ALCOHOL DETOX AT HOME Detoxing from alcohol at home isn’t recommended. If you’re a regular or heavy alcohol user and you stop drinking without the help of a medical professional, you’re at risk for a number of complications from alcohol withdrawal symptoms. The severity of these alcohol withdrawal symptoms depends on factors like: If you quit alcohol “cold turkey” and have an alcohol addiction or dependency, symptoms of alcohol withdrawal may start as soon as six hours after your last drink. Alcohol abuse and alcoholism teaches your brain that operating on alcohol is normal. When you quit drinking, your brain and central nervous system go into high alert to restore balance. In regular and heavy drinkers, the body compensates for the depressive effects of alcohol by increasing hormones and brain chemicals, such as: When you quit alcohol cold turkey, your body becomes flooded with abnormally high levels of these chemicals. This is the brain’s way of trying to restore balance and normal functioning without alcohol. That’s why quitting cold turkey can put you at risk for alcohol withdrawal symptoms like: 1. Seizures Alcohol withdrawal seizures are sometimes the first sign of alcohol withdrawal. They involve convulsions alternating with involuntary muscle contractions. Withdrawal seizures can occur within 6 to 48 hours of stopping alcohol consumption. 2. Delirium Tremens (DTs) About 30% to 40% of people who experience seizures get the DTs. Severe symptoms like the DTs typically occur 24 to 48 hours after the last drink and are characterized by: Without medical help, the DTS can put you at risk for: 3. Abnormal Heart Rhythms As part of delirium tremens, the heart beats erratically. Unusual shifts in breathing, temperature, and circulation may contribute to a racing heart. You may also experience blood circulation issues like high blood pressure. 4. Nausea and Vomiting Symptoms like nausea and vomiting may linger for around a week after you stop drinking. Like other alcohol withdrawal symptoms, these issues result from your brain trying to rebalance neurotransmitters without alcohol. 5. Dehydration Alcohol is a diuretic that increases your urine output and may also increase sweating. You may already be dehydrated going into alcohol withdrawal. During alcohol withdrawal, you can get even more dehydrated due to vomiting and diarrhea. These can cause dangerous electrolyte imbalances that affect the central nervous system, causing: Other alcohol withdrawal symptoms may include: Alcohol detox at home is dangerous. The best way to safely detox from alcohol is under the care of medical professionals. They can help you deal with withdrawal symptoms using research-backed medications and other approaches as appropriate. They can also immediately attend to any medical emergencies. RISKS OF DRUG DETOX AT HOME In addition to alcohol detox at home, drug detox at home can also come with a number of complications. It can be uncomfortable and dangerous, and it can set you up for relapse. Drug addiction has a high relapse rate because it’s a chronic disease. Drug detox at home can bring on intense drug cravings that make it nearly impossible to refrain from using drugs. Withdrawal symptoms make returning to drug use seem like a good idea just to ease your discomfort. Quitting drugs cold turkey can cause dangerous withdrawal symptoms within a few hours of your last dose as your brain works to find balance. The progression of withdrawal and risks of drug detox at home depends on: 1. Type of Drug The type of drug abuse makes a difference during drug detox. The following drugs are considered highly addictive with potentially serious withdrawal symptoms: 2. Length and Severity of Drug Abuse The larger doses of drugs you use at a time and the more often you use them, the more your brain and body depends on the substance. The higher the level of dependence, the more intense withdrawal will be. 3. Co-Occurring Disorders and Medical Conditions Medical conditions can complicate drug withdrawal. For instance,





